For Pharma Companies

Solving the Challenges of Product Reach and Patient Support
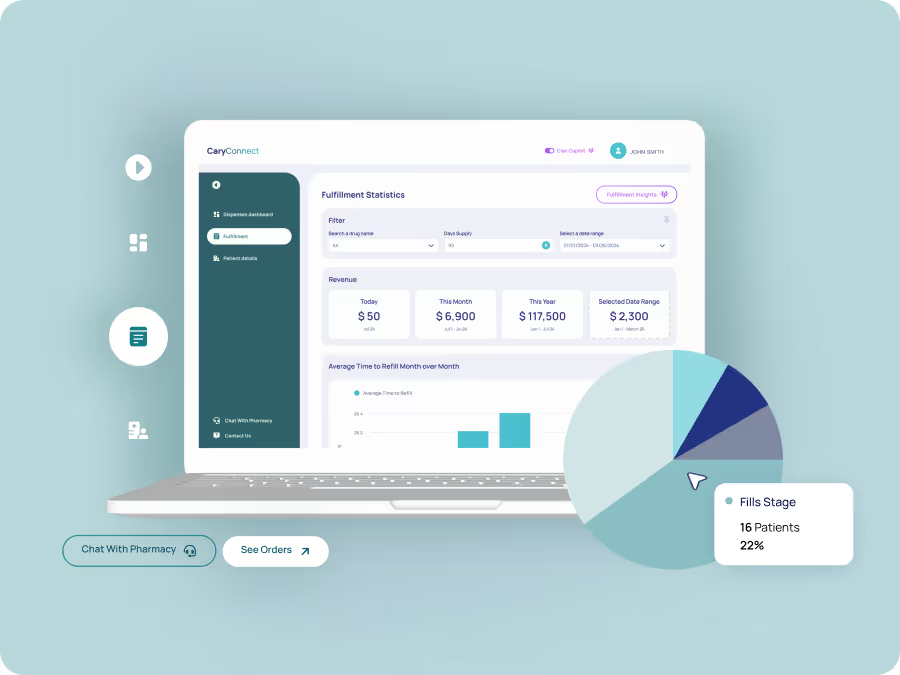
Limited visibility into prescription fulfillment and patient access hinders Pharma Manufacturers and Telehealth organizations from evaluating product performance and optimizing delivery.
CaryConnect’s innovative API provides the insights and tools needed to eliminate bottlenecks, streamline distribution, and enhance patient engagement for better outcomes.
Explore


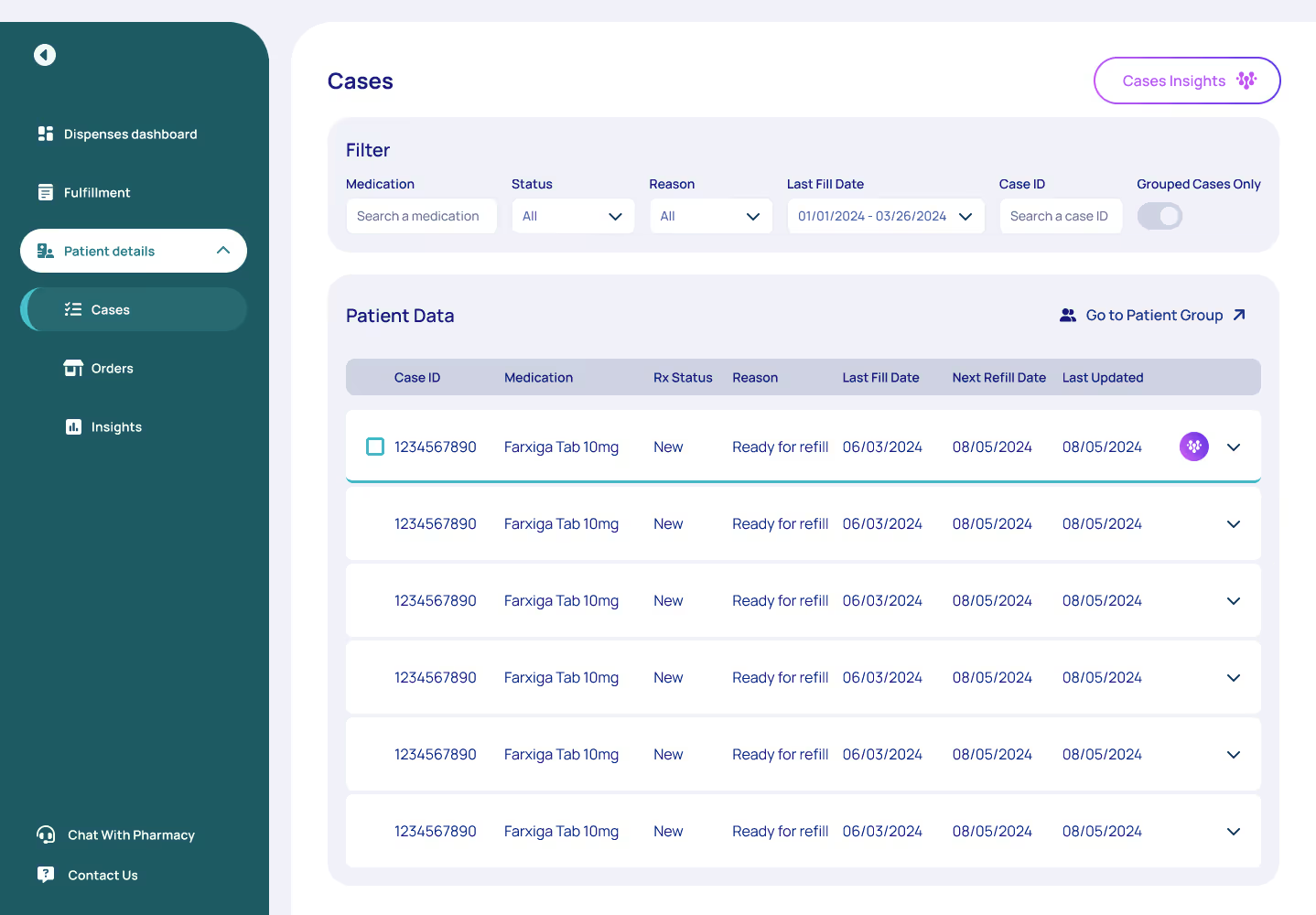
Real-Time Prescription Insights

Benefits Investigation Made Simple

Nationwide Access & Payment Solutions

Customizable API for Scalable Distribution